Volume 9, Issue 2 (Summer 2023)
JMIS 2023, 9(2): 168-179 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Zareii P, Meraji M, Mazloum S R, Yousefi M, Fazaeli S. Effectiveness of Feedback Method in Improving the Nursing Documentation in the Emergency Department of Imam Reza Hospital in Mashhad, Iran. JMIS 2023; 9 (2) :168-179
URL: http://jmis.hums.ac.ir/article-1-426-en.html
URL: http://jmis.hums.ac.ir/article-1-426-en.html
Department of Health Information Technology, School of Paramedical and Rehabilitation Sciences, Mashhad University of Medical Sciences, Mashhad, Iran.
Full-Text [PDF 4941 kb]
(1001 Downloads)
| Abstract (HTML) (1710 Views)
Full-Text: (1700 Views)
Introduction
According to the laws, all the activities and patient care of medical staff must be recorded and documented. Lack of report or any error in providing these reports can lead to legal convictions. Therefore, hospitals should identify and improve the factors that increase the quality of documentation. However, research conducted in most countries indicates the low quality of nursing documentation. Research for evaluation of emergency departments of hospitals in Iran has shown that not only documentation standards are not met in most cases, but also many services provided to the patient are not even recorded in the files. This can make the emergency department (ED) far from a standard unit, in addition to financial damage to the hospital. Therefore, interventions such as holding educational workshops, continuous and planned monitoring, and audit & feedback have been used to improve the behavior and performance of those responsible for documentation in health care centers. Considering the importance of nursing documentation, especially in the emergency department, this study aims to evaluate the status of nursing documentation before and after providing feedback to nurses in the ED of a hospital in Mashhad, Iran.
Methods
This is a quasi-experimental study that was conducted in 2022 in the emergency department of Imam Reza Hospital in Mashhad City. At first, to design an evaluation tool for the ED nursing documentation, all articles published until the end of 2020 in Farsi and English were searched in reliable databases using the keywords nurse, documentation, file, emergency (in both Persian and English). Finally, 27 related articles were selected to extract nursing documentation indicators. Then, the extracted indicators were given to 12 experts in the field of nursing and health information management who had experience in documentation studies to check their validity. At this stage, the items that obtained the acceptable CVR and CVI values were selected. The internal consistency method was used for determining the reliability of the tool. In the next step, 150 medical records were randomly selected from among the ED cases in Imam Reza Hospital and examined by the designed tool (with 18 items). In the third stage, the results of assessing the current status of ED nursing documentation along with the guideline for correct documentation were given to the nurses as feedback in a video format. Then, one month after examining the status of nursing documentation, 150 medical records of discharged patients were evaluated. In the final stage, the data related to the evaluations carried out in both stages before and after giving feedback were analyzed in SPSS software, version 22 using independent t-test, chi-square test, and Fisher’s exact statistical test.
Results
The CVR and CVI of 18 items of the designed tool had values above 0.56 and 0.79, respectively. The internal consistency using Cronbach’s α was obtained 0.85 which was acceptable. According to Table 1, the mean score of nursing documentation status obtained for 150 cases was 27.9±2.1 in the pre-test phase (ranged 21.4-32.6) and 29.1±1.6 in the post-test phase (ranged 25.9±31.8) out of 36.
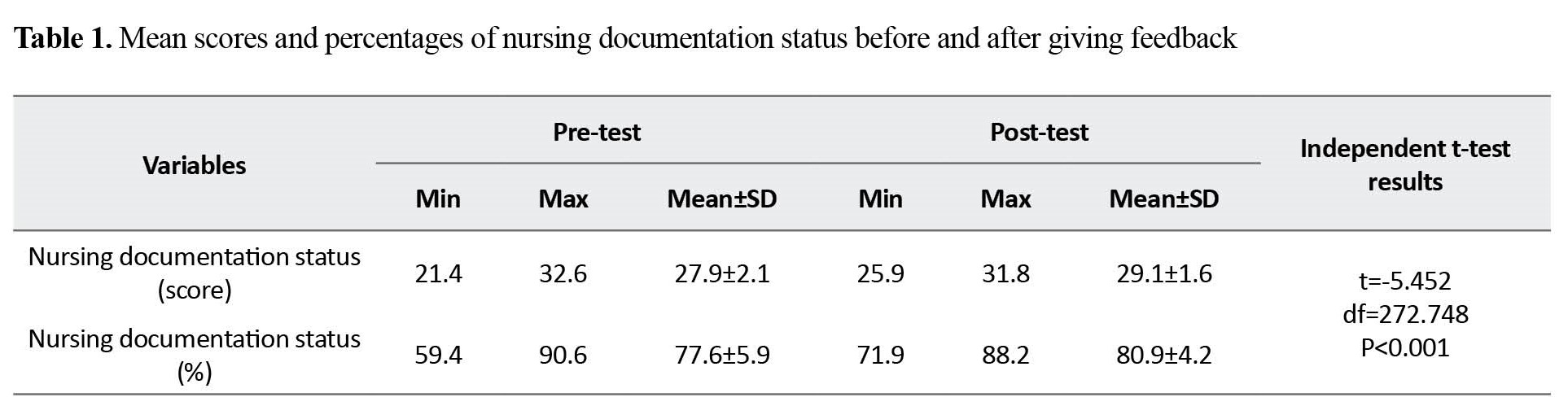
In overall, the comparison of the mean scores showed that the ED nursing documentation status increased significantly after giving feedback to the nurses (P<0.001).
Conclusion
The result of the psychometric analysis of the designed tool showed that it had good reliability and validity to be used in examining the status of nursing documentation in the EDs. The status of ED nursing documentation was at a good level both before and after giving feedback to the nurses. It was significantly increased after giving feedback. The highest percentage of complete documentation of cases in both stages (before and after feedback) were related to adherence to the time sequence between nursing reports, adherence to the use of a pen with blue or black ink, and registration of vital signs in the vital sign control form according to the sequence requested by the physician in a legible and accurate manner. The highest percentage of incomplete documentation in both stages was related to the triage form and compliance with the principles of correction or addition.
Considering the existence of defects in medical records and the importance of documentation in improving nursing services and providing optimal services to patients, it is recommended to use the feedback method to improve nursing documentation in the EDs. It is recommended to regularly evaluate the nursing documentation status and provide positive or negative feedback to nurses and other interested groups based on the quality of the documentation and compliance with nursing documentation indicators.
Ethical Considerations
Compliance with ethical guidelines
The protocol of this project has been approved by the Ethics Committee of the Mashhad University of Medical Sciences (Code: IR.MUMS.REC.1399.34).
Funding
This research was taken from MSc thesis's of Parisa Zareii, approved by Department of Health Information Technology and Medical Records, Mashhad University of Medical Sciences (Code no.981278).
Authors' contributions
Conceptualization: Somayeh Fazaeli, Parisa Zareii; Methodology, resources, investigation, review & editing: All author, Writing the original draft: Somayeh Fazaeli and Parisa Zareii; Funding acquisition: Somayeh Fazaeli; Supervision: Somayeh Fazaeli and Marzieh Meraji.
Conflicts of interest
The authors declared no conflict of interests.
Acknowledgements
The authors hereby express their gratitude to the respected head of the health information technology unit and the head of the emergency department and other respected colleagues of the health information management department at Imam Reza Hospital who cooperated with us in collecting data.
References
According to the laws, all the activities and patient care of medical staff must be recorded and documented. Lack of report or any error in providing these reports can lead to legal convictions. Therefore, hospitals should identify and improve the factors that increase the quality of documentation. However, research conducted in most countries indicates the low quality of nursing documentation. Research for evaluation of emergency departments of hospitals in Iran has shown that not only documentation standards are not met in most cases, but also many services provided to the patient are not even recorded in the files. This can make the emergency department (ED) far from a standard unit, in addition to financial damage to the hospital. Therefore, interventions such as holding educational workshops, continuous and planned monitoring, and audit & feedback have been used to improve the behavior and performance of those responsible for documentation in health care centers. Considering the importance of nursing documentation, especially in the emergency department, this study aims to evaluate the status of nursing documentation before and after providing feedback to nurses in the ED of a hospital in Mashhad, Iran.
Methods
This is a quasi-experimental study that was conducted in 2022 in the emergency department of Imam Reza Hospital in Mashhad City. At first, to design an evaluation tool for the ED nursing documentation, all articles published until the end of 2020 in Farsi and English were searched in reliable databases using the keywords nurse, documentation, file, emergency (in both Persian and English). Finally, 27 related articles were selected to extract nursing documentation indicators. Then, the extracted indicators were given to 12 experts in the field of nursing and health information management who had experience in documentation studies to check their validity. At this stage, the items that obtained the acceptable CVR and CVI values were selected. The internal consistency method was used for determining the reliability of the tool. In the next step, 150 medical records were randomly selected from among the ED cases in Imam Reza Hospital and examined by the designed tool (with 18 items). In the third stage, the results of assessing the current status of ED nursing documentation along with the guideline for correct documentation were given to the nurses as feedback in a video format. Then, one month after examining the status of nursing documentation, 150 medical records of discharged patients were evaluated. In the final stage, the data related to the evaluations carried out in both stages before and after giving feedback were analyzed in SPSS software, version 22 using independent t-test, chi-square test, and Fisher’s exact statistical test.
Results
The CVR and CVI of 18 items of the designed tool had values above 0.56 and 0.79, respectively. The internal consistency using Cronbach’s α was obtained 0.85 which was acceptable. According to Table 1, the mean score of nursing documentation status obtained for 150 cases was 27.9±2.1 in the pre-test phase (ranged 21.4-32.6) and 29.1±1.6 in the post-test phase (ranged 25.9±31.8) out of 36.
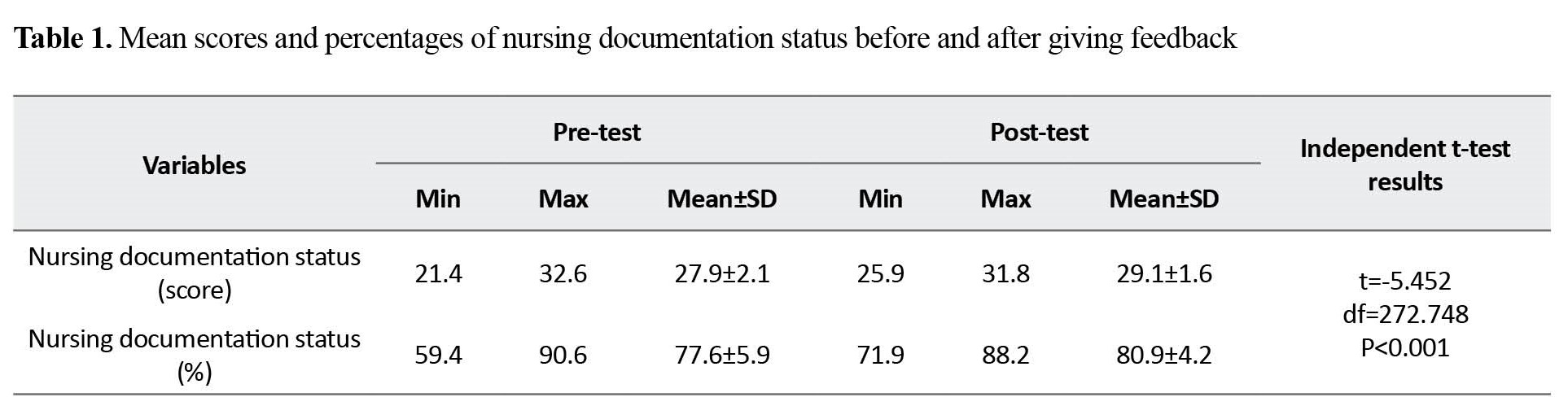
In overall, the comparison of the mean scores showed that the ED nursing documentation status increased significantly after giving feedback to the nurses (P<0.001).
Conclusion
The result of the psychometric analysis of the designed tool showed that it had good reliability and validity to be used in examining the status of nursing documentation in the EDs. The status of ED nursing documentation was at a good level both before and after giving feedback to the nurses. It was significantly increased after giving feedback. The highest percentage of complete documentation of cases in both stages (before and after feedback) were related to adherence to the time sequence between nursing reports, adherence to the use of a pen with blue or black ink, and registration of vital signs in the vital sign control form according to the sequence requested by the physician in a legible and accurate manner. The highest percentage of incomplete documentation in both stages was related to the triage form and compliance with the principles of correction or addition.
Considering the existence of defects in medical records and the importance of documentation in improving nursing services and providing optimal services to patients, it is recommended to use the feedback method to improve nursing documentation in the EDs. It is recommended to regularly evaluate the nursing documentation status and provide positive or negative feedback to nurses and other interested groups based on the quality of the documentation and compliance with nursing documentation indicators.
Ethical Considerations
Compliance with ethical guidelines
The protocol of this project has been approved by the Ethics Committee of the Mashhad University of Medical Sciences (Code: IR.MUMS.REC.1399.34).
Funding
This research was taken from MSc thesis's of Parisa Zareii, approved by Department of Health Information Technology and Medical Records, Mashhad University of Medical Sciences (Code no.981278).
Authors' contributions
Conceptualization: Somayeh Fazaeli, Parisa Zareii; Methodology, resources, investigation, review & editing: All author, Writing the original draft: Somayeh Fazaeli and Parisa Zareii; Funding acquisition: Somayeh Fazaeli; Supervision: Somayeh Fazaeli and Marzieh Meraji.
Conflicts of interest
The authors declared no conflict of interests.
Acknowledgements
The authors hereby express their gratitude to the respected head of the health information technology unit and the head of the emergency department and other respected colleagues of the health information management department at Imam Reza Hospital who cooperated with us in collecting data.
References
- Ala A, Moharamzadeh P, Pouraghaei M, Almasi A, Mashrabi O, Jafarlou V. Designing a model for medical documentation as per joint commission international in emergency department of Tabriz Imam Reza Hospital. Int J Curr Res Aca Rev. 2014; 2(10):72-80. [Link]
- Ahmadi O, Ghazi Talkhoncheh M, Pirnia Naieni A, Tansaz Z. [Quality of nursing care and documentation with overcrowding in emergency department (Persian)]. Iran J Emerg Med. 2016; 3(2):53-7. [DOI:10.22037/ijem.v3i2.9975]
- Mousavi A, Yousefi M, Jamali J, Meraji M, Fazaeli S. [Design and implementation of tools for rapid assessment of the status of documentation of emergency department’physicians (Persian)]. J Mod Med Inf Sci. [DOI:10.52547/jmis.7.4.52]
- Kimiafar K, Vafaee Najar A, Sarbaz M. [Quantitative investigation of inpatients’ medical records in training and social security hospitals in Mashhad (Persian)]. J Paramed Sci Rehabil. 2015; 4(1):58-67. [DOI:10.22038/JPSR.2015.4068]
- Ahmadi M, Gorzin Z, Khoshgam M. [Nurses needs assessment on methods of documentation in electronic health records (Persian)]. Hakim J. 2013; 16(3):251-7. [Link]
- Gorzin Z, Ahmadi R, Samadbeik M. [Opportunities and challenges electronic health records documentation from the perspective of nurses (Persian)]. J Clin Res Paramed Sci. 2016; 4(4):e82065. [Link]
- Sohrabi Z, Loni S, Taavoni S. [Determining the educational needs of emergency nurses in educational hospitals of Iran, Tehran, and Shahid Beheshti Universities of Medical Sciences through Delphi technique, 2013 (Persian)]. Iran J Med Educ. 2014; 14(5):448-64. [Link]
- Broderick MC, Coffey A. Person-centred care in nursing documentation. Int J Older People Nurs. 2013; 8(4):309-18. [DOI:10.1111/opn.12012] [PMID]
- Jasemi M, Mohajal Aghdam A, Rahmani A, Abdollahzadeh F, Zamanzadeh V. [Assessing quality of nursing documentations and effective factors on it in medical-surgical units (Persian)]. J Nurs Manag. 2012; 1(3):37-45. [Link]
- Dehghani M, Hayavie Haghighi MH, Tayary N, Khorami F. [Nurses’ organizational behavior and their quality of documentation (Persian)]. J Nurs Educ. 2015; 3(4):68-80. [Link]
- Esmailian M, Nasr-Esfahani M, Brahimi AS. [The quality of patients’ files documentation in emergency department; a cross sectional study (Persian)]. Iran J Emerg Med. 2014; 1(1):16-21. [DOI:10.22037/ijem.v1i1.7178]
- Lorenzetti DL, Quan H, Lucyk K, Cunningham C, Hennessy D, Jiang J, et al. Strategies for improving physician documentation in the emergency department: A systematic review. BMC Emerg Med. 2018; 18(1):36. [DOI:10.1186/s12873-018-0188-z] [PMID] [PMCID]
- Vafaei SM, Manzari ZS, Heydari A, Froutan R, Farahani LA. Nurses’ perception of nursing services documentation barriers: A qualitative approach. Electron J Gen Med. 2018; 15(3):em28. [DOI:10.29333/ejgm/86184]
- Meidani Z, Farzandipour M, Davoodabadi A, Farrokhian A, Kheirkhah D, Sharifi M, et al. Effect of reinforced audit and feedback intervention on physician behaviour: A multifaceted strategy for targeting medical record documentation. J R Coll Physicians Edinb. 2017; 47(3):237-42. [DOI:10.4997/jrcpe.2017.305] [PMID]
- Vafaei SM, Manzari ZS, Heydari A, Froutan R, Farahani LA. Improving nursing care documentation in emergency department: A participatory action research study in Iran. Open Access Maced J Med Sci. 2018; 6(8):1527-32. [DOI:10.3889/oamjms.2018.303] [PMID] [PMCID]
- Sadoughi F, Meidani Z, Farzandipour M, Davoodabadi A, Farrokhian A, Gilasi H. [The effect of feedback and incentive mechanisms on improving residents’ medical record documentation procedure (Persian)]. Iran J Med Educ. 2015; 15:648-55. [Link]
- Karami M, Shokrizadeh Arani L. [Related factors in medical records documentation quality and presenting solutions from managers’ and physicians’ viewpoints occupied in hospitals affiliated to Kashan University of Medical Sciences (Persian)]. Iran J Med Educ. 2010; 9(4):356-64. [Link]
- Arzamani M, Doulatabadi T, Hashemi M. [Effect of training on the degree of completeness of medical records in the hospitals of North Khorasan University of Medical Sciences in Bojnurd (Persian)]. J North Khorasan Univ Med Sci. 2011; 3(1):15-21. [DOI:10.29252/jnkums.3.1.2]
Type of Study: Research |
Subject:
Special
Received: 2022/10/15 | Accepted: 2023/02/13 | Published: 2023/07/1
Received: 2022/10/15 | Accepted: 2023/02/13 | Published: 2023/07/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |








 hums.ac.ir
hums.ac.ir