Volume 9, Issue 4 (Winter 2024)
JMIS 2024, 9(4): 330-339 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Barati A, Mirmohammadkhani M, Ghods S, Moshiri E. Effective Factors in Improving the Family Physician Referral System in Bojnord, Iran. JMIS 2024; 9 (4) :330-339
URL: http://jmis.hums.ac.ir/article-1-481-en.html
URL: http://jmis.hums.ac.ir/article-1-481-en.html
Social Determinants of Health Research Center, Semnan University of Medical Sciences, Semnan, Iran.
Full-Text [PDF 3628 kb]
(163 Downloads)
| Abstract (HTML) (292 Views)
Full-Text: (53 Views)
Introduction
The referral system is a comprehensive organizational framework in which various institutions are well defined and specified based on their responsibilities and authority. In a successful referral, health care facilities should be accessible to all and the staff should be well trained to provide quality health services and be able to provide essential equipment, supplies and medicines. The comprehensive referral system has been successfully implemented in developed countries and its disadvantages have been eliminated to a large extent; however, these systems are still evolving, updating, and changing from paper-based to digital systems in developing countries and have challenges for deployment and sustainable use. Identifying the influencing factors (barriers and facilitators) in the development of the family physician referral system is very important, since it ultimately leads to the promotion of justice in the distribution of health services and the improvement of society’s satisfaction. Iran is one of the countries whose health system has undergone many changes due to many threats and opportunities.
The referral system in Iran has been established for several years with the aim of improving the distribution of health care services and is being updated to be more efficient. Considering that a detailed evaluation of the performance of the family physician referral system has not been done in Iran and the factors affecting the referral system have not been well investigated, this study aims identify indicators and main components in improving the family physician referral system in Bojnord, Iran.
Methods
This is a quantitative-qualitative study that was conducted in 2021in Bojnord City. First the components of the study were extracted using face-to-face interviews with 24 experts (qualitative phase). The entry criteria for the experts were consent to participate in the study, familiarity with the health referral system in Bojnord City, and having at least 8 years of management experience in the field of referral and health systems in Bojnord City. In the next step, the initial version of a researcher-made questionnaire (with 27 items) was created and used to collect the experts’ opinions. The scoring was based on a 5-point Likert scale. Its reliability using Cronbach’s α, was obtained 0.9, which was acceptable. Next, the fuzzy hierarchical analysis was used to identify the most important factors (quantitative phase). In this study, to identify the importance of components by experts, each component was compared with another component.
Results
Organizational/managerial requirements, human resource management requirements, and information technology requirements were extracted and compared with each other (Table 1).
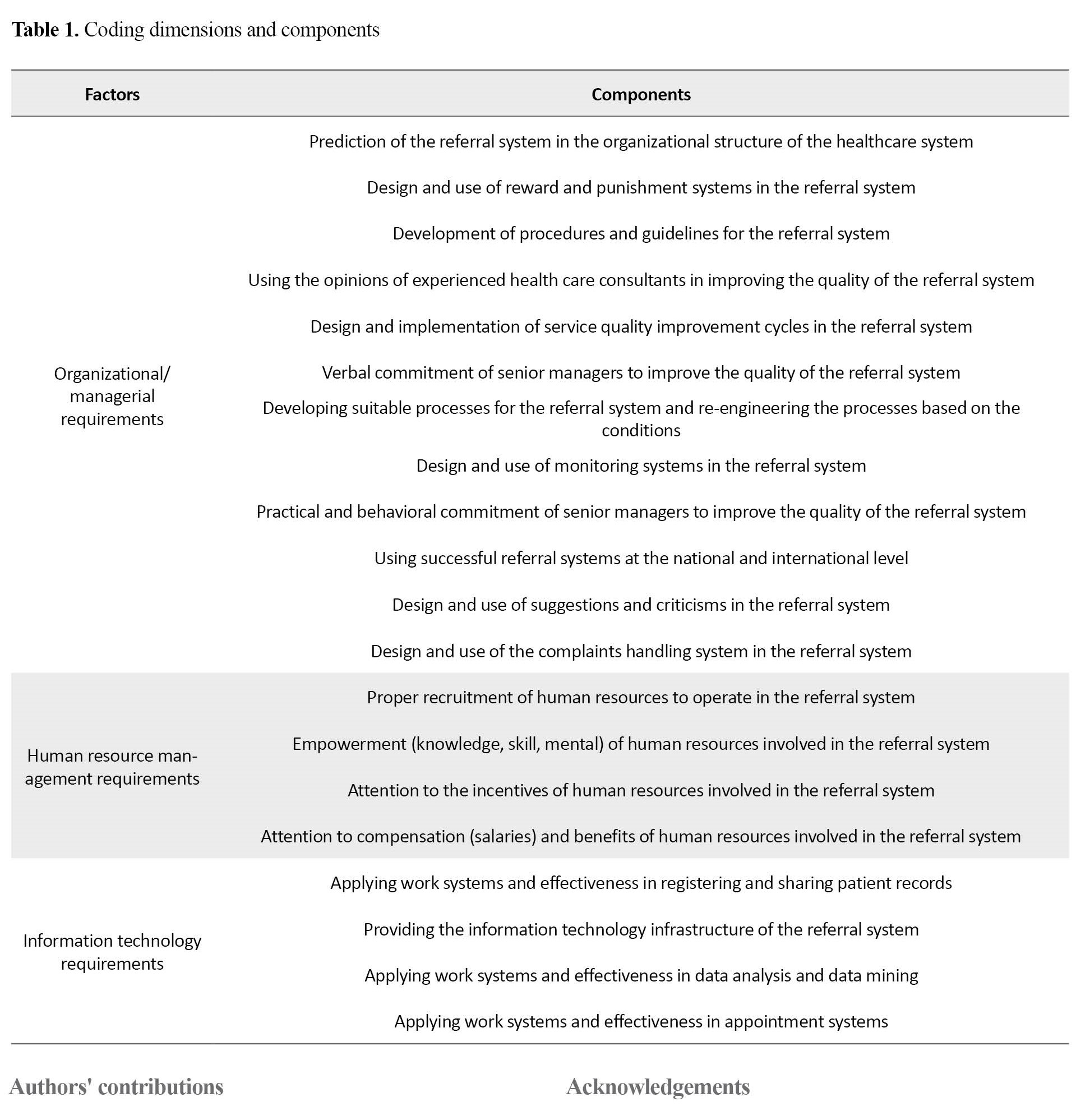
It was found that the organizational/managerial requirements had the most importance, followed by technological and human resource management requirements. Among the organizational/managerial requirements, the component “using the opinions of experienced health care consultants in improving the quality of the referral system” had the highest importance. Among the human resources management requirements, the component “empowerment (knowledge, skill, mental) of human resources involved in the referral system” had the highest importance. Finally, among the information technology requirements, “providing the information technology infrastructure of the referral system” had the highest importance.
Conclusion
The use of clear and simplified procedures and rules, improvement of facilities to move towards the digitalization of the referral system, along with the staff training seems to play a significant role in improving the family physician referral system in Bojnord City. The identified components can be used as indicators in other cities of Iran. Therefore, it is recommended that further studies be conducted because various factors such as social, economic, and cultural differences may change the importance and even the form of the components.
Ethical Considerations
Compliance with ethical guidelines
This research was assessed and approved by the Ethic Research Committee of Islamic Azad University, Semnan Branch (Code: IR.IAU.SEMNAN.REC.1399.025).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and investigation: Alireza Barati and Esmaeil Moshiri; Software: Samaneh Ghods, Alireza Barati; Formal analysis: Samaneh Ghods, Alireza Barati and Esmaeil Moshiri; The original draft preparation: Alireza Barati, Esmaeil Moshiri and Majid Mirmohammadkhuni; Methodology, review and editing: All authors.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors thank and appreciate of Bojnord University of Medical Sciences and Islamic Azad University, Semnan Branch, for their support.
References
The referral system is a comprehensive organizational framework in which various institutions are well defined and specified based on their responsibilities and authority. In a successful referral, health care facilities should be accessible to all and the staff should be well trained to provide quality health services and be able to provide essential equipment, supplies and medicines. The comprehensive referral system has been successfully implemented in developed countries and its disadvantages have been eliminated to a large extent; however, these systems are still evolving, updating, and changing from paper-based to digital systems in developing countries and have challenges for deployment and sustainable use. Identifying the influencing factors (barriers and facilitators) in the development of the family physician referral system is very important, since it ultimately leads to the promotion of justice in the distribution of health services and the improvement of society’s satisfaction. Iran is one of the countries whose health system has undergone many changes due to many threats and opportunities.
The referral system in Iran has been established for several years with the aim of improving the distribution of health care services and is being updated to be more efficient. Considering that a detailed evaluation of the performance of the family physician referral system has not been done in Iran and the factors affecting the referral system have not been well investigated, this study aims identify indicators and main components in improving the family physician referral system in Bojnord, Iran.
Methods
This is a quantitative-qualitative study that was conducted in 2021in Bojnord City. First the components of the study were extracted using face-to-face interviews with 24 experts (qualitative phase). The entry criteria for the experts were consent to participate in the study, familiarity with the health referral system in Bojnord City, and having at least 8 years of management experience in the field of referral and health systems in Bojnord City. In the next step, the initial version of a researcher-made questionnaire (with 27 items) was created and used to collect the experts’ opinions. The scoring was based on a 5-point Likert scale. Its reliability using Cronbach’s α, was obtained 0.9, which was acceptable. Next, the fuzzy hierarchical analysis was used to identify the most important factors (quantitative phase). In this study, to identify the importance of components by experts, each component was compared with another component.
Results
Organizational/managerial requirements, human resource management requirements, and information technology requirements were extracted and compared with each other (Table 1).
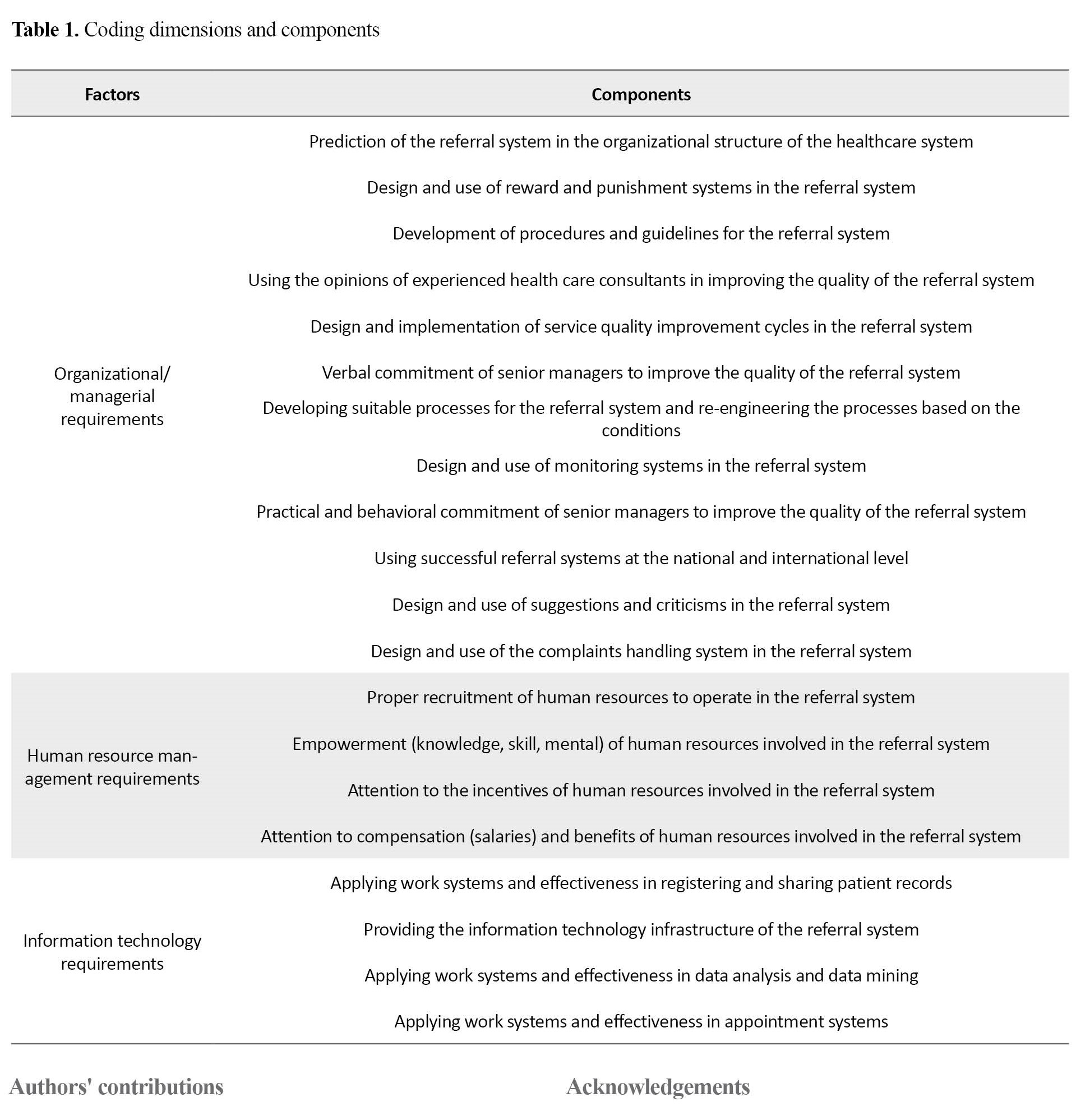
It was found that the organizational/managerial requirements had the most importance, followed by technological and human resource management requirements. Among the organizational/managerial requirements, the component “using the opinions of experienced health care consultants in improving the quality of the referral system” had the highest importance. Among the human resources management requirements, the component “empowerment (knowledge, skill, mental) of human resources involved in the referral system” had the highest importance. Finally, among the information technology requirements, “providing the information technology infrastructure of the referral system” had the highest importance.
Conclusion
The use of clear and simplified procedures and rules, improvement of facilities to move towards the digitalization of the referral system, along with the staff training seems to play a significant role in improving the family physician referral system in Bojnord City. The identified components can be used as indicators in other cities of Iran. Therefore, it is recommended that further studies be conducted because various factors such as social, economic, and cultural differences may change the importance and even the form of the components.
Ethical Considerations
Compliance with ethical guidelines
This research was assessed and approved by the Ethic Research Committee of Islamic Azad University, Semnan Branch (Code: IR.IAU.SEMNAN.REC.1399.025).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and investigation: Alireza Barati and Esmaeil Moshiri; Software: Samaneh Ghods, Alireza Barati; Formal analysis: Samaneh Ghods, Alireza Barati and Esmaeil Moshiri; The original draft preparation: Alireza Barati, Esmaeil Moshiri and Majid Mirmohammadkhuni; Methodology, review and editing: All authors.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors thank and appreciate of Bojnord University of Medical Sciences and Islamic Azad University, Semnan Branch, for their support.
References
- Nguru K, Ireri L. Challenges influencing proper implementation of quality health care referral system in Kaloleni Sub-county, Kilifi County in Kenya. Int Emerg Nurs. 2022; 62:101169. [DOI:10.1016/j.ienj.2022.101169] [PMID]
- Tabrizi JS, Karamouz M, Sadeghi-Bazargani H, Nikniaz A, Nikniaz L, Hasanzadeh R, et al. Health complex model as the start of a new primary healthcare reform in Iran: Part B: The intervention protocol. Iran J Public Health. 2019; 48(1):147. [DOI:10.18502/ijph.v48i1.803]
- Damari B, Heidari A, Rahbari Bonab M, Vosoogh Moghadam A. Designing a toolkit for the assessment of Health in All Policies at a national scale in Iran. Health Promot Perspect. 2020; 10(3):244-9. [DOI:10.34172%2Fhpp.2020.38] [PMID] [PMCID]
- Kabir MJ, Delgoshaei B, Vatankhah S, Ravaghei H, Jafari N, Heidari A, et al. Determinant criteria for designing health benefit package in selected countries. Life Scie J. 2013; 10(3):1392-403. [Link]
- Sokhanvar M, Kabir MJ, Bevrani H, Nosratnejad S, Janati A, Hasanpoor E. Family physician and referral system adherence in Iranian primary healthcare system. Fam Med Prim Care Rev. 2020; 22(2):158-65. [DOI:10.5114/fmpcr.2020.95325]
- Hughes CA, Allen P, Bentley M. eReferrals: Why are we still faxing? Aust J Gen Pract. 2018; 47(1-2):50-7. [DOI:10.31128/AFP-07-17-4285] [PMID]
- Naseriasl M, Janati A, Amini A, Adham D. Referral system in rural Iran: Improvement proposals. Cad Saude Publica. 2018; 34(3):e00198516. [DOI:10.1590/0102-311X00198516] [PMID]
- Kalroozi F, Mohammadi N, Farahani MA, Aski BH, Anari AM. A critical analysis of Iran health system reform plan. J Educ Health Promot. 2020; 9:364. [DOI:10.4103/jehp.jehp_493_20] [PMID] [PMCID]
- Reza Khankeh H, Bagheri Lankarani K, Zarei N, Joulaei H. Three decades of healthcare system reform in Iran from the perspective of universal health coverage: A macro-qualitative study. Iran J Med Sci. 2021; 46(3):198-206. [PMID] [PMCID]
- Xiao Y, Chen X, Li Q, Jia P, Li L, Chen Z. Towards healthy China 2030: Modeling health care accessibility with patient referral. Soc Sci Med. 2021; 276:113834. [DOI:10.1016/j.socscimed.2021.113834] [PMID]
- Outland BE, Erickson S, Doherty R, Fox W, Ward L; Medical Practice and Quality Committee of the American College of Physicians, et al. Reforming physician payments to achieve greater equity and value in health care: A position paper of the american college of physicians. Ann Intern Med. 2022; 175(7):1019-21. [DOI:10.7326/M21-4484] [PMID]
- Tajari F, Mahmoudi G, Dabbaghi F, Yazdani-Charati J. Designing a model for evaluating the performance of electronic patient referral system in the healthcare system of Iran. Iran Red Crescent Med J. 2022; 24(8):e2089. [DOI:10.32592/ircmj.2022.24.8.2089]
- Talebpour M, Hadadi A, Oraii A, Ashraf H. Rationale and design of a registry in a referral and educational medical center in Tehran, Iran: Sina Hospital Covid-19 registry (SHCo-19R). Front Emerg Med. 2020; 4(2s):e53. [DOI:10.22114/ajem.v0i0.361]
- Amir-Behghadami M, Janati A. Iranian national COVID-19 electronic screening system: Experience to share. Emerg Med J. 2020; 37(7):412-3. [DOI:10.1136/emermed-2020-209806] [PMID] [PMCID]
- Doshmangir L, Bazyar M, Majdzadeh R, Takian A. So near, so far: Four decades of health policy reforms in Iran, achievements and challenges. Arch Iran Med. 2019; 22(10):592. [Link]
- Olyaeemanesh A, Behzadifar M, Mousavinejhad N, Behzadifar M, Heydarvand S, et al. Iran's health system transformation plan: A SWOT analysis. Med J Islam Repub Iran. 2018; 32:39. [DOI:10.14196%2Fmjiri.32.39] [PMID] [PMCID]
- Hsu LM, Ding JF. Applying the fuzzy analytic hierarchy process method to evaluate key indicators of health promotion policies for the elderly in Taiwan. J Healthc Eng. 2021; 2021:4832877. [DOI:10.1155/2021/4832877] [PMID] [PMCID]
- Haider S, Ahmad J, Ahmed M. Identifying barriers to implementation of health promoting schools in Pakistan: The use of qualitative content analysis and fuzzy analytic hierarchy process. Int J Adv Appl Sci. 2018; 5(4):56-66. [DOI:10.21833/ijaas.2018.04.007]
- Handayani PW, Saladdin IR, Pinem AA, Azzahro F, Hidayanto AN, Ayuningtyas D. Health referral system user acceptance model in Indonesia. Heliyon. 2018; 4(12):e01048. [DOI:10.1016/j.heliyon.2018.e01048] [PMID] [PMCID]
- Azamar-Alonso A, Costa AP, Huebner LA, Tarride JE. Electronic referral systems in health care: A scoping review. Clinicoecon Outcomes Res. 2019; 11:325-33. [DOI:10.2147/ceor.s195597] [PMID] [PMCID]
- Zhang X, Wang T, Yu Y, Zhao S. Key nodes affecting patient satisfaction in a cross-regional referral service process: An empirical analysis study in Sichuan. BMC Health Serv Res. 2018; 18(1):840. [DOI:10.1186/s12913-018-3460-8] [PMID] [PMCID]
- Tully KP, Gibson AN, Pearsall MS, Umstead K, Gill C, Stuebe AM. Screening and referral for social determinants of health: Maternity patient and health care team perspectives. Health Equity. 2022; 6(1):887-97. [DOI:10.1089/heq.2022.0020] [PMID] [PMCID]
- Esan O, Oladele O. Referral letters to the psychiatrist in Nigeria: Is communication adequate? Afr Health Sci. 2016; 16(4):1023-6. [DOI:10.4314/ahs.v16i4.19] [PMID] [PMCID]
- Zhang Z, Liu S, Xiang M, Li S, Zhao D, Huang C, et al. Protecting healthcare personnel from 2019-nCoV infection risks: Lessons and suggestions. Front Med. 2020; 14(2):229-31. [PMID]
- Han ER, Yeo S, Kim MJ, Lee YH, Park KH, Roh H. Medical education trends for future physicians in the era of advanced technology and artificial intelligence: An integrative review. BMC Med Educ. 2019; 19(1):460. [DOI:10.1186/s12909-019-1891-5] [PMID] [PMCID]
- Seyed-Nezhad M, Ahmadi B, Akbari-Sari A. Factors affecting the successful implementation of the referral system: A scoping review. J Family Med Prim Care. 2021; 10(12):4364-75. [DOI:10.4103%2Fjfmpc.jfmpc_514_21] [PMID] [PMCID]
- Martins J, Branco F, Gonçalves R, Au-Yong-Oliveira M, Oliveira T, Naranjo-Zolotov M, et al. Assessing the success behind the use of education management information systems in higher education. Telematics Inform. 2019; 38:182-93. [DOI:10.1016/j.tele.2018.10.001]
- Lu C, Zhang Z, Lan X. Impact of China's referral reform on the equity and spatial accessibility of healthcare resources: A case study of Beijing. Soc Sci Med. 2019; 235:112386. [DOI:10.1016/j.socscimed.2019.112386] [PMID]
- Stewart J, Krows ML, Schaafsma TT, Heller KB, Brown ER, Boonyaratanakornkit J, et al. Comparison of racial, ethnic, and geographic location diversity of participants enrolled in clinic-based vs 2 remote COVID-19 clinical trials. JAMA Netw Open. 2022; 5(2):e2148325. [DOI:10.1001/jamanetworkopen.2021.48325] [PMID] [PMCID]
Type of Study: Research |
Subject:
General
Received: 2023/08/21 | Accepted: 2023/12/20 | Published: 2024/01/1
Received: 2023/08/21 | Accepted: 2023/12/20 | Published: 2024/01/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |








 hums.ac.ir
hums.ac.ir